Psoriasis Tissue Model
Human 3D (NHu-3D) Psoriasis Tissue Model
NEW Organotypic Model for Pre-clinical Drug Screening!
- Human 3D Model of Psoriatic Tissue
- Fully Differentiated, Ready-To-Use
- Unsurpassed Tissue Reproducibility
- Quantifiable, Objective Endpoints
- Cost Effective Pre-clinical Drug Testing
Drug Discovery, Development, Delivery & Toxicology Tools
Standardized Human 3D in vitro Tissue Models
Attribute
- Ki67
- HBD2
- Psoriasis
- Elafin
- Calgranulin C
- Cytokeratin 16
- And More
- IL-6
- IL-8
- GM-CSF
- And More
The Psoriasis Tissue Model is responsive to treatment with anti-psoriatic compounds in a dose dependent manner.
Features
Psoriasis Tissue Model
- Psoriatic Human Tissue Phenotype
- 3-Dimensional, Highly Differentiated
- Serum-Free Media System
- Highly Reproducible
- Easily-handled Cell Culture Inserts
- Quantifiable, Objective Endpoints
- Ideal for Drug Screening and Basic Studies
- Cost Effective Alternative to Animal and Clinical Testing
General MatTek Tissue Features
- Unsurpassed Long-Term Tissue Reproducibility
- 3-Dimensional, Highly Differentiated Tissue
- Metabolically, Mitotically Active
- Produced from Normal (Non-Transformed) Human Cells - Ideal for Genomics Studies
- Produced in Easily Handled Cell Culture Inserts
- Grown in Completely Serum-Free Media System
- Quantifiable, Objective Test Endpoints
- Cost Effective Alternative to Animal and Human Clinical Testing
Applications
Psoriasis Tissue Model
- Anti-Psoriatic Drug Screening
- Basic Psoriatic Research
Data Sheet
Psoriasis is a chronic inflammatory skin disease characterized by epidermal hyperplasia (Acanthosis) with elongated ridges and abnormal differentiation of epidermal keratinocytes, dermal angiogenesis, abnormal accumulation of polymorphonuclear leukocytes, infiltration of activated T cells and dendritic cells (DC), and increased cytokine levels. To enable in vitro study of psoriasis and screen therapeutic candidates for safety and efficacy, MatTek has developed an organotypic psoriasis tissue model (SOR-300-FT).
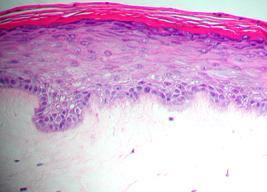
The psoriasis tissue model is cultured using normal human epidermal keratinocytes and psoriatic fibroblasts harvested from psoriasis lesions (Figs. 1A and 1B). The cells are cultured on specially prepared cell culture inserts using serum free medium to form a multilayered, highly differentiated tissue. The SOR-300-FT tissues adopt a psoriatic phenotype as evidenced by increased basal cell proliferation, expression of psoriasis-specific markers (Fig. 4), and elevated release of cytokines related to psoriasis (Fig. 5). Morphologically, the tissue model closely parallels lesional psoriatic human tissues. This model provides researchers with a useful, in vitro means to assess the safety and efficacy of lead therapeutic compounds and to study other basic psoriasis biology phenomena.

Figure 1: H&E stained histological (formalin fixed) cross-sections of: A) in vitro reconstructed psoriasis tissue model (SOR-300-FT) containing normal human keratinocytes and psoriatic fibroblasts, and B) psoriasis-involved skin explants.
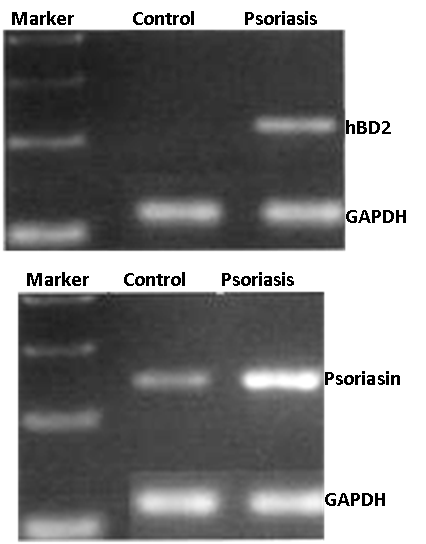
Figure 2: RT-PCR showing upregulation of the antimicrobial peptides human β-defensin-2 (hBD2) and psoriasin by the psoriasis (SOR-300-FT) and normal human skin (EFT-300-FT) models.
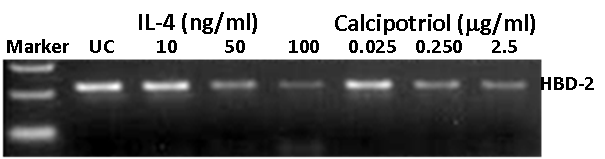
Figure 3: RT-PCR results showing effect of different concentrations of IL-4 and calcipotriol on HBD-2 expression in the psoriatic tissue model (SOR-300-FT). Marker = 100-bp ladder; UC = untreated psoriatic tissue model.
The psoriasis tissue model (SOR-300-FT) exhibits a psoriatic phenotype as evidenced by increased expression of psoriasis-associated markers including human β-defensin-2 (HBD2) (Fig. 2), psoriasin (Fig. 2), SKALP/elafin (Fig. 4), activated STAT3, keratinocyte hyperproliferative cells (Ki67 staining (Fig. 4) and proinflammatory cytokines/ chemokines such as IL-6, IL-8, GM-CSF, and IP-10 (Fig. 5).
Various drug development and toxicology laboratories are actively seeking alternatives to expensive clinical or whole animal testing. The availability of a relevant psoriasis model will serve as a tool to study drug candidate toxicity, cutaneous cellular and molecular biology features of psoriasis, cell-cell interactions, and keratinocyte responses. Figure 3 shows that calcipotriol, a common anti-psoriasis agent, reduces HBD2 expression. Such an assay, along with other straightforward protocols, can be used to predict the responsiveness and irritancy of new psoriasis drug formulations.
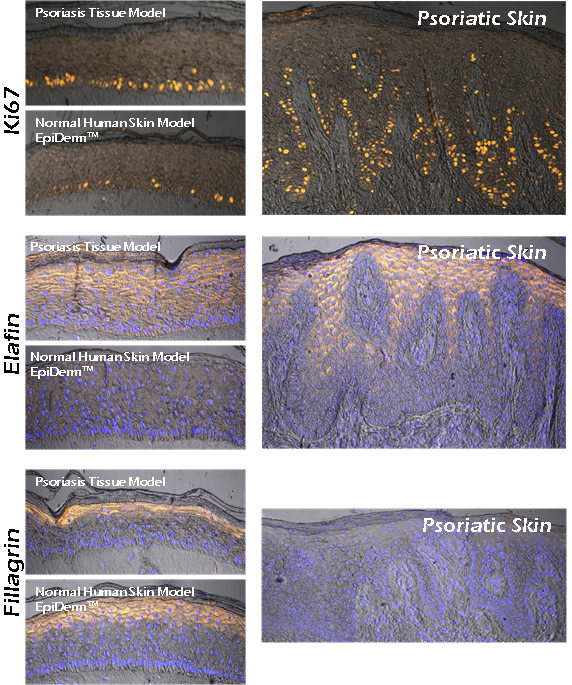
Figure 4: Immunohistochemistry showing expression of psoriasis associated markers by the psoriasis model (SOR-300-FT) and psoriasis explant tissues. Shown: Increased basal cell proliferation (Ki67), increased expression of elafin, and decreased expression of filaggrin.
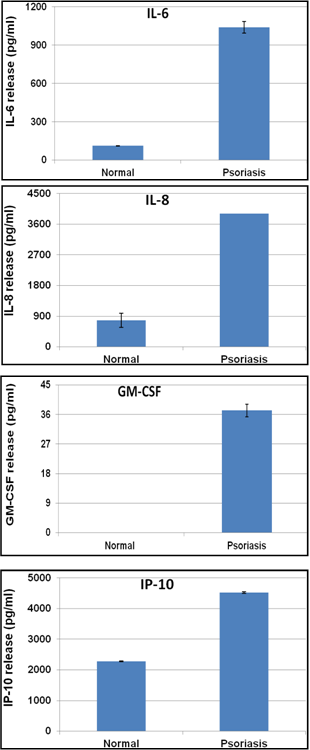
Figure 5: ELISA results showing cytokine release levels by psoriasis tissue (SOR-300-FT) versus normal human skin model (EpiDerm-FT).
Technical References
702. DEVELOPMENT AND CHARACTERIZATION OF 3D PSORIATIC TISSUE MODEL.
Summary:
Psoriasis is an inflammatory skin disease marked by hyperproliferation and abnormal keratinocyte differentiation that affects about 2% of the global population. In this study, we developed a human cell based in vitro psoriatic tissue model from psoriatic fibroblasts and normal keratinocytes using an optimized serum-free culture medium. When compared to normal skin reconstructs, confocal microscopic evaluation of stained psoriatic tissue reconstructs revealed: 1) hyperproliferation of basal epithelial cells (Ki67), 2) increased STAT 3, and elafin expression, 3) reduced levels of filaggrin, and 4) similar pattern of cytokeratin 10 expression to that of the normal skin reconstruct. RT-PCR analysis of the psoriatic tissue model also showed overexpression of HBD-2, psoriasin, elafin, and neutrophil chemotactic cytokines such as growth-related oncogene alpha (GROα), interleukin-8 (IL-8), and epithelial cell derived neutrophil-activating peptide 78 (ENA-78). Similar to the in vivo situation, cytokine analysis of culture supernatants from the psoriatic tissue model showed increased release of IL-6 (9 fold), IL-8 (5.9 fold), and IP-10 (2 fold) when compared to normal reconstructed epidermal tissues. Topical exposure of the psoriatic tissue to the therapeutic agent calcipotriol hydrate showed a dose dependent decrease in HBD-2 and psoriasin gene expression by 2000 and 380 fold, respectively. In conclusion, the psoriatic tissue model mimics its in vivo counterpart in terms of tissue morphology, structure, gene expression (human beta defensin 2, psoriasin, and elafin), and cytokine release (IL-6, IL-8, GM-CSF). Availability of a well- characterized in vitro psoriatic tissue model will be a valuable tool to study the biology of psoriasis, enhance understanding of the disease, and accelerate the development of therapeutic candidates.
______________________________________________________________________________________________________
Keywords: Calgranulin A, Calgranulin B, Calgranulin C, Cytokeratin 10, Effector proteins, Elafin, ENA-78, Epithelial cell derived neutrophil-activating peptide 78 (ENA-78), Filaggrin, GCP-2, GM-CSF, GROα, Human beta defensin-2, Human beta defensin-3, Hyperproliferation, IL-6, IL-8, Interleukin-8, IP-10, IP-9, Ki67, LL-37, MIP-3a, Psoriasin, Psoriasis, Psoriasis model, Secretory Leukocyte Peptidase Inhibitor, SOR-300-FT, STAT 3, TLR2, Transglutaminase
Materials Tested: Calcipotriol hydrate
_______________________________________________________________________________________________________________________
본 Paper에 대한 문의는 상담실에서 하시면 됩니다. 상담실바로가기
701. DELPHINIDIN INDUCES EPIDERMAL DIFFERENTIATION AND INHIBITS PROLIFERATION AND INFLAMMATION IN A THREE-DIMENSIONAL RECONSTITUTED SKIN MODEL OF PSORIASIS.
Summary:
Psoriasis is a chronic, inflammatory skin disease characterized by epidermal hyperproliferation and aberrant keratinocyte differentiation. Several lines of evidence suggest that intrinsic alterations of the epidermis may play an important role in the pathogenesis of psoriasis. Identification of natural agents that possess the ability to abrogate these effects could be useful for the treatment of this disease. Delphinidin, present in pigmented fruits and vegetables, possesses potent antioxidant and anti-inflammatory activities. In this study, we examined the effect of delphinidin on markers of epidermal differentiation, proliferation and inflammation by employing three-dimensional models of reconstituted normal and psoriatic human skin. Delphinidin (5-20 μM; 2-8 days) treatment of reconstituted human skin increased the processing of caspase-14, protein expression of transglutaminase-1, involucrin, loricrin and filaggrin in a dose- and time-dependent manner. In addition, delphinidin treatment induced terminal differentiation resulting in more rapid formation of cornified envelopes without inducing apoptosis. Next, studies were performed to establish the significance of these findings by employing a three-dimensional reconstituted skin model of psoriasis. Psoriasis is characterized by down-regulation of differentiation markers, including caspase-14 and filaggrin, and by upregulation of markers of proliferation (Ki67 and PCNA) and inflammation (iNOS) in the epidermis. Employing immunohistochemical analysis, we found that treatment of psoriatic tissues with delphinidin resulted in an increased expression of caspase-14 and filaggrin. In addition, delphinidin treatment reduced these markers of cell proliferation and inflammation. We suggest that delphinidin could be a promising agent for treatment of psoriasis.
______________________________________________________________________________________________________
Keywords: Anthocyanidin, Caspase-14, Cell proliferation, Filaggrin, Inflammation, iNOS, Ki67, Loricrin, PCNA, Procaspase-3, Procaspase-8, Procaspase-9, proliferation, Psoriasis, Psoriatic human skin model, Psoriatic tissue models (PTM), SOR-300-FT, Transglutaminase 1
Material Tested: Delphinidin
_______________________________________________________________________________________________________________________
본 Paper에 대한 문의는 상담실에서 하시면 됩니다. 상담실바로가기






< Anti-Psoriasis Drug Screening
www.MatTek.co.kr